Connecting Primary and Virtual Care: Providers’ Perspectives on Achieving Seamless Integration
A Qualitative Study Summary by Omada Health + Stanford Healthcare AI Applied Research Team (HEA3RT)
This edition covers:
- Primary care providers' views on virtual care adoption
- Challenges and considerations of utilizing virtual care
- Opportunities to bolster the partnership between virtual care and conventional healthcare systems
Studies have shown that virtual care programs are effective, complementary solutions for chronic disease management, yielding improved clinical outcomes (e.g., better blood pressure control) and reduced costs of medical care. While such research is promising and demonstrates the benefits of virtual care, additional research is warranted to explore seamless collaboration between primary care and virtual care services to enhance clinical outcomes. To learn more, Omada Health collaborated with Stanford's HEA3RT team to conduct the first round of a two-phase qualitative study to better understand providers’ perspectives on the acceptability, utility, barriers and opportunities associated with virtual care programs.
What We Learned
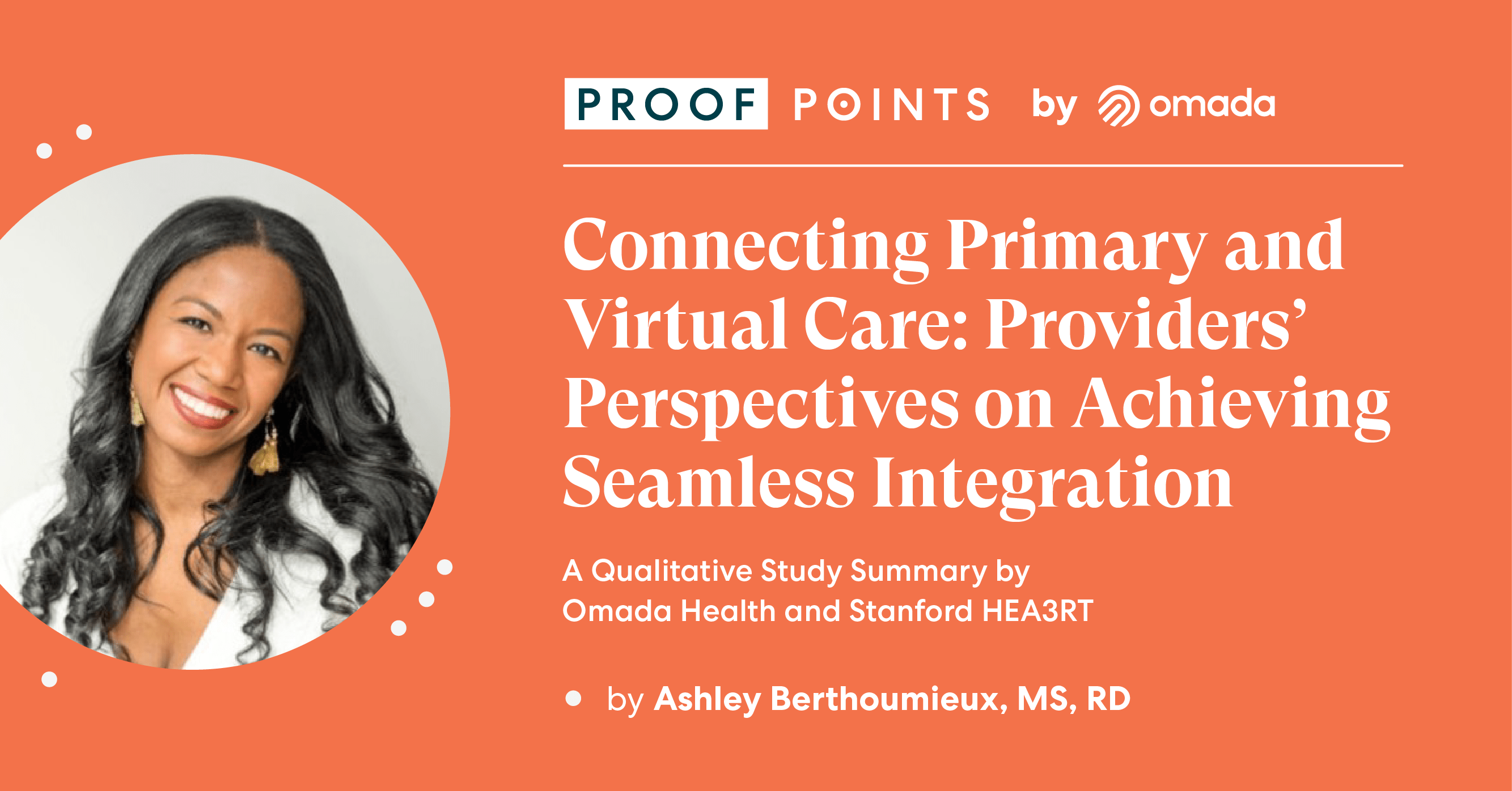
Providers Value Virtual Care
Findings from this study indicate that the majority of the providers sampled (76%) were confident about recommending digital health programs to their patients, with levels of confidence ranging from moderately to extremely confident [Figure 1].
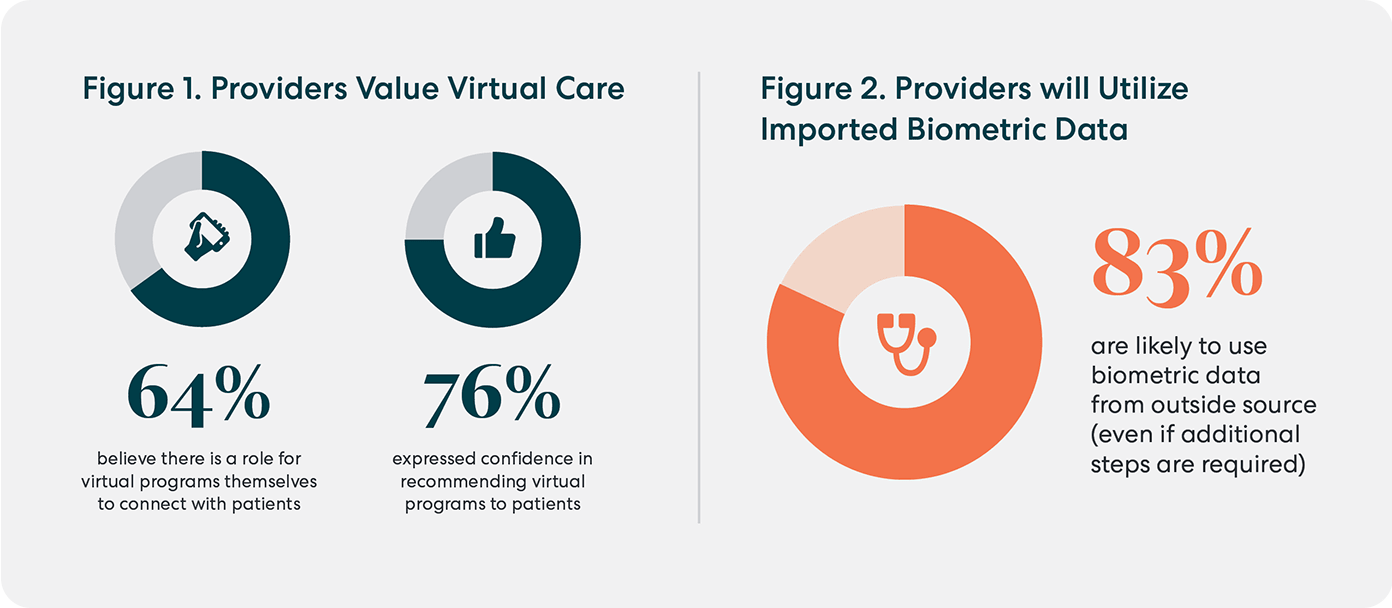
They’re Big on Biometric Data
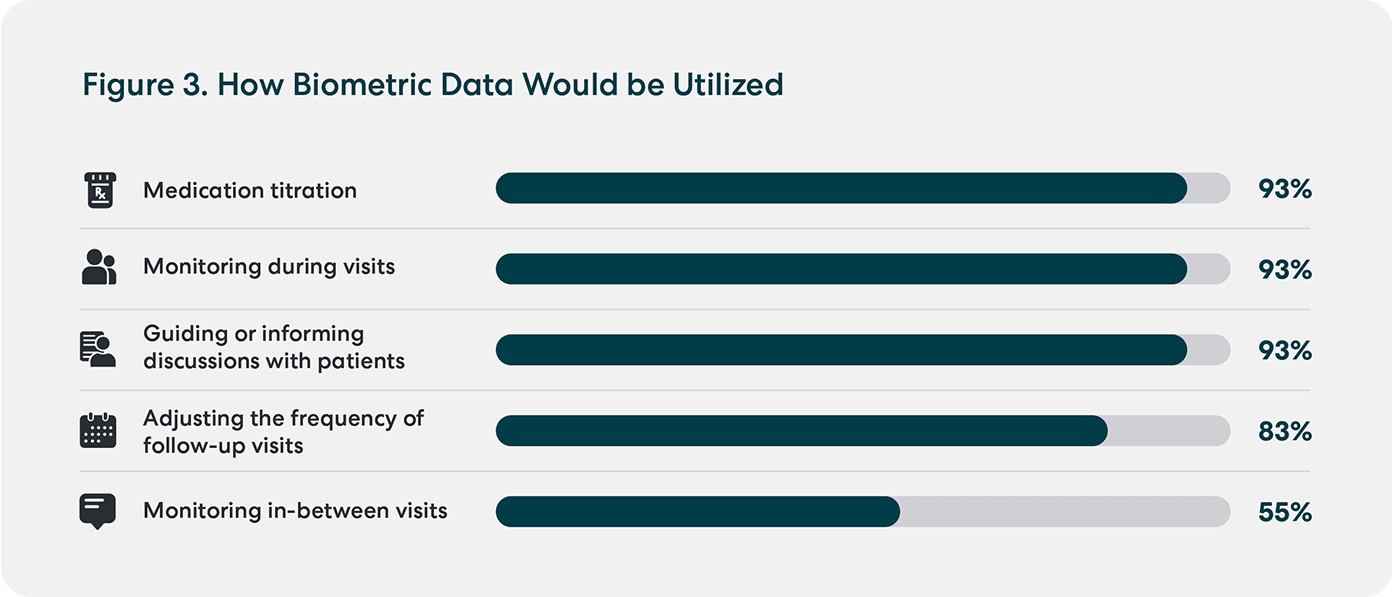
The majority of those surveyed (83%) expressed they would be very/extremely likely to use biometric data (e.g. weight, blood glucose, and blood pressure) from an outside source during a visit, if it were imported into a patient’s electronic health record (EHR), despite needing extra clicks or steps to access the report [Figure 2]. Over 90% of providers conveyed that they would refer to the data primarily for medication titration, monitoring during visits, and directing discussions with patients [Figure 3].
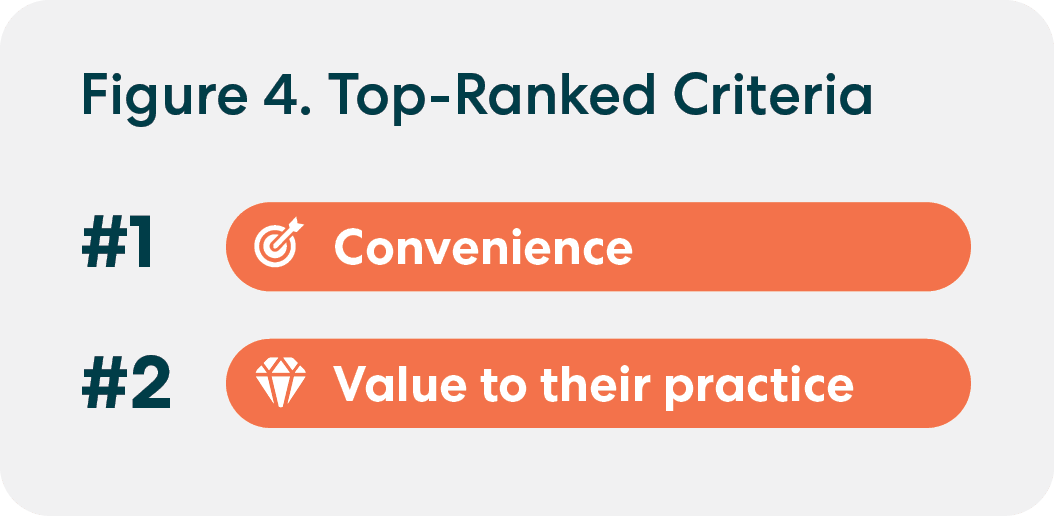
Convenience and Curation Drive Value
“Provider’s convenience” and “value to my practice” were participants’ top-ranked criteria for exchanging data with virtual care programs and incorporating it into patient care, highlighting the importance of practical considerations alongside data integration [Figure 4].
Additionally, while 76% of providers indicated that they would not want to be notified each time their patients’ biometric data or summary reports from outside sources are uploaded to Epic™–the EHR utilized at Stanford Health Care–those interested in that feature offered recommendations for streamlining the process. Their suggestions included presenting the data regularly on a set schedule, for abnormal values only, and/or right before an upcoming patient visit.
An Eye on Equity
Virtual health care offers many opportunities to improve the quality of patient care by transforming the traditional paradigm of medicine with the use of tools such as artificial intelligence/machine learning (AI/ML), mobile apps, wearable devices, and telehealth.
However, a digital divide exists among those who have access to the technology and those who don’t. Affordability and location significantly contribute to the divide, particularly affecting people living in "digital deserts"—areas with little to no internet access—thereby hindering their ability to participate in telehealth and virtual care services. This issue is compounded by systemic biases in healthcare that promote disparities in the quality of care and health outcomes among historically marginalized communities in the U.S., including patients who are women, Black, Indigenous, and People of Color (BIPOC), Lesbian, Gay, Bisexual, Transgender, Queer/Questioning, Intersex, Asexual and others (LGBTQIA+), living with disabilities, and/or non-English speakers.
PCPs were encouraged to share additional feedback on virtual care at the end of the study survey in an open-ended response. They revealed concerns surrounding health equity and the prohibitive costs of programs, particularly focusing on communities affected by healthcare disparities.
One provider said, “I worry about equity and access for these programs and patients who historically underutilized technology in medicine.”
Another added, “I hope we can provide patients with free digital devices for blood pressure and blood glucose monitoring that connect with the electronic medical record.”
These insights emphasize the need to ensure access and affordability in delivering virtual care, promoting inclusivity among patients and confidence among providers in using these services.
“The things that are important include access, reliability, safety of data, and equity of these programs… We need to ensure that these programs are not widening disparities.” - Primary Care Physician
Challenges and Considerations
While most PCPs are willing to recommend digital health programs to their patients, they shared concerns during interviews about insufficient program knowledge and the complexities of exchanging and utilizing data from outside sources that may use different EHR platforms.
Providers’ Top Concerns Regarding Virtual Care
- Continuity of Care
- Equity Concerns
- Data Overload and Time Burden
- Lack of Program Knowledge/Provider Education
- Cost Concerns
- Referral Burden
Building Bridges Between Virtual and Primary Care
Findings from this study suggest that there are substantial opportunities to bolster the partnership between virtual care and conventional healthcare systems, especially as it relates to efficient data exchange. Seamless and bidirectional communication between virtual care providers and primary care teams has the potential to improve healthcare quality, safety, and clinical outcomes.
Overall, the study’s findings identified three key strategies to promote collaboration with healthcare providers: 1) seamless interoperability between digital health platforms and EHRs at large health systems 2) the strategic and secure use of AI/ML to help reduce providers’ workloads and facilitate referrals to virtual care programs, and 3) health equity measures built into virtual care delivery to improve access and affordability.
Looking ahead, the responsible integration of AI/ML technologies could optimize interoperability between EHRs at large health systems and virtual care platforms by streamlining data exchange and referral processes. This collaboration demonstrates the value of engaging with providers and health systems to realize the value of virtual care solutions in patient care, while further developing the technology needed to advance integration. Understanding the facilitators and barriers associated with the adoption of virtual care data in primary care practice helps refine communication with providers and better support their patients in between clinic visits. To build upon these efforts, ongoing collaboration, implementation, and evaluation strategies will continue to strengthen our programs.
To learn more, read the full whitepaper here.
