3 Reasons Behavior Change Support is Vital to Obesity Care
By Carmen Kaperick, LICSW, CDCES
This edition covers:
- Why GLP-1s are not a silver bullet for obesity
- The role of behavior change support teams and how they complement obesity medicine specialists
- How providers can work in concert to achieve optimal outcomes
It’s becoming increasingly clear that GLP-1s are a breakthrough, but not a silver bullet for long-term weight health. In fact, one study found that 58% of all individuals who used GLP-1s for weight management stopped treatment within three months, and gaining weight after discontinuation is common. Individuals taking GLP-1s for weight loss can also experience issues like shame and lack of social support.
While these trends are not ideal, they can help guide obesity care providers on how to best support patients in achieving sustained weight health. This lies in addressing behaviors related to diet, exercise, sleep, mental health, and social drivers of health. However, doing so may not be the primary focus of obesity medicine specialists.
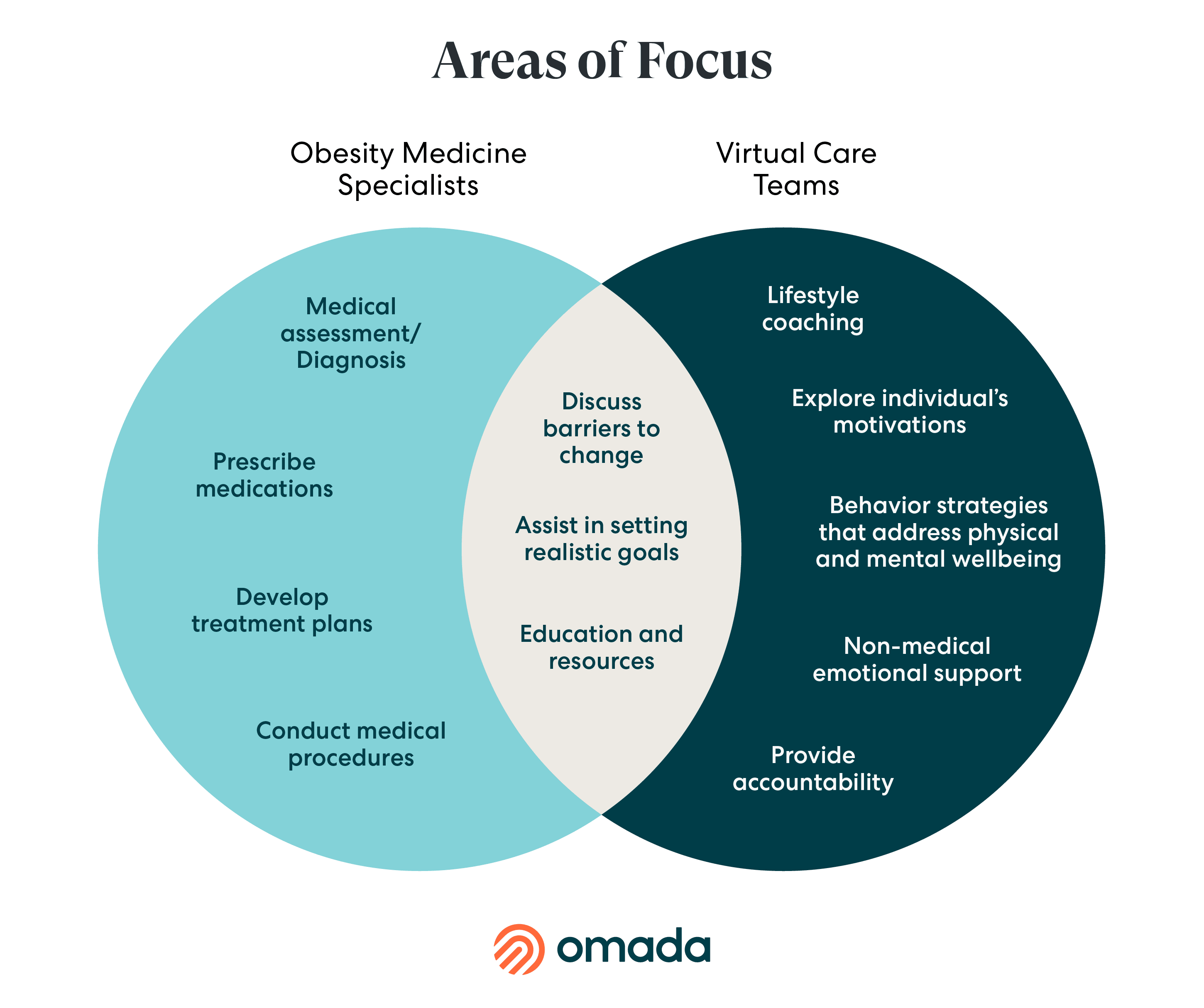
Obesity medicine specialists mainly prioritize the medical elements of care (i.e. diagnosing conditions and prescribing medications), and may not have sufficient touch points or bandwidth to address day-to-day behavior change support. Virtual care teams that focus on behavior change (i.e. health coaches, condition specialists, physical activity coaches and social workers), on the other hand, are specifically trained to fill these gaps.
Given this important distinction, here are the top three reasons why behavior change support is vital to obesity care.
1. Behavior Change Support Focuses on Intrinsic Motivation, not just Extrinsic Motivation
In exploring the various specialties that assist with weight loss, understanding the difference between extrinsic and intrinsic motivation is crucial. Extrinsic motivators often revolve around external goals set by professionals, such as: "I need to reduce my sugar intake because my doctor advised it."
Following medical advice is an extrinsic motivation. At the same time, decades of behavior change science tells us that people do best with intrinsic motivation, which delves into personal aspirations and reasons, such as: "I'm doing this for myself because I want to play with my grandkids."
Virtual care teams focus on intrinsic motivation by addressing habits, emotional and social factors, and can help patients explore their values and goals, facilitating a personal drive for change.
There are a few reasons why obesity specialists may focus on extrinsic motivators, as opposed to more intrinsic motivators in obesity care:
Time Constraints
Within their constrained timeframe, obesity specialists are often focused on diagnosing conditions, prescribing treatments, and managing immediate health concerns, rather than exploring patient's motivations for change.
Background
Their training and focus traditionally emphasizes clinical diagnostics and treatment plans over emphasizing lifestyle behavior change support in the period between office visits.
Healthcare System Pressures
Obesity specialists may, at times, be pressured to focus on quantitative outcomes and efficiency. They may operate under the assumption that their role is primarily authoritative, believing that patients should be compliant with prescriptions and advice given.
2. Behavior Change Support Turns “Why” into “How”
With a virtual care team that focuses on behavior change support, patients can identify those intrinsic motivators that make losing weight feel personal, meaningful and deeply fulfilling.
Behavior change support can empower patients to feel in control of their health, rather than solely focusing on a certain number on a scale.
Virtual care teams take a patient’s “why” and help them realize the ensuing “how.” That means helping patients understand their strengths and barriers. For example, behavior change support can help patients understand their unique relationship with food and how to develop healthier ways to cope with difficult emotions. This type of support can lead to “aha” moments and translate into realistic, actionable plans to develop better coping strategies.
At Omada, we have seen how behavior change support can help individuals on their journey, particularly with:
Goal-Setting
Virtual care teams can help establish health goals in collaboration with patients, and stay invested through regular check-ins, accountability, motivation, stress management and plateau handling. Omada members who set goals with their care teams are 2.5x as likely to achieve target outcomes vs. members who do not.
Self-Monitoring/Tracking
Helping to track and celebrate progress is another critical part of behavior change support. Care team feedback on logged meals, at the right time, helps improve Omada members’ meal tracking by 10-15%.
Relationship Building
Virtual care teams can help motivate and build strong relationships with patients. Omada members who actively engage with their care teams experience twice the weight loss compared to those who do not. With care teams in their corner, members are equipped with emotional, informational, and practical support.
3. Behavior Change Support Infuses Joy into the Weight Health Journey
Obesity is a complex chronic condition and the process of getting healthier is often a journey. Along the way, individuals are much more likely to stick with it if they enjoy the process.
Yes, that’s right; joy can play a pivotal role in weight health.
Behavior change support focuses on setting goals and adopting strategies that align with each individual member’s culture, values and lifestyle. In other words, virtual care teams don’t seek to change who members are, only what health behaviors they engage in. They don’t focus on restrictive measures like diet mentality that can lead to feelings of guilt, self-blame, irritation and anxiety, as well as fatigue and attention problems. For example, chronic dieters may perpetually feel as though they’ve messed up, which decreases self-esteem and makes them feel increasingly like passengers instead of pilots on their health journey.
Holistic Obesity Care Helps Drive Outcomes
Primary care providers, obesity medicine specialists and virtual care teams focused on behavior change support work best in concert, rather than in competition with one another.
While obesity medicine specialists help diagnose and treat obesity, virtual care teams help individualize patient care and promote conversations about mindful eating, physical activity and mental health barriers.
This complementary approach appears to drive notable outcomes. Recent analyses of Omada’s Enhanced GLP-1 Care Track saw members adopting health-promoting behaviors and achieving healthy weight loss, and those in a GLP-1 discontinuation path experienced -0.1% average weight change at 4 months after stopping their GLP-1 use.
By developing rapport and leading with empathy, virtual care teams meet members where they are and get their hands dirty, so to speak, in the aim of addressing the health behaviors that lead to long-term weight health.
