New Indications, Promising Outcomes, and Third-Party Prescribing

Omada Health’s Guide to GLP-1s | Q1 - Q2 2025
As the GLP-1 conversation evolves, Omada Health is updating its industry FAQs to deliver timely data and insights for virtual care buyers.
In 2024, we focused on weight loss quality vs. quantity, usage and costs, off-ramping protocols, and equity issues. We also drilled into emerging details of the GLP-1 experience, including compounded GLP-1s, how to manage the medication’s impact on body composition, and ways to assess the value of virtual companion programs.
In this guide, we address new indications and their impact on employers and payers, as well as early outcomes of Omada’s Enhanced GLP-1 Care Track, and primary care perspectives on third-party telehealth prescribers.
New Indications Build Pressure on Employers and Payers
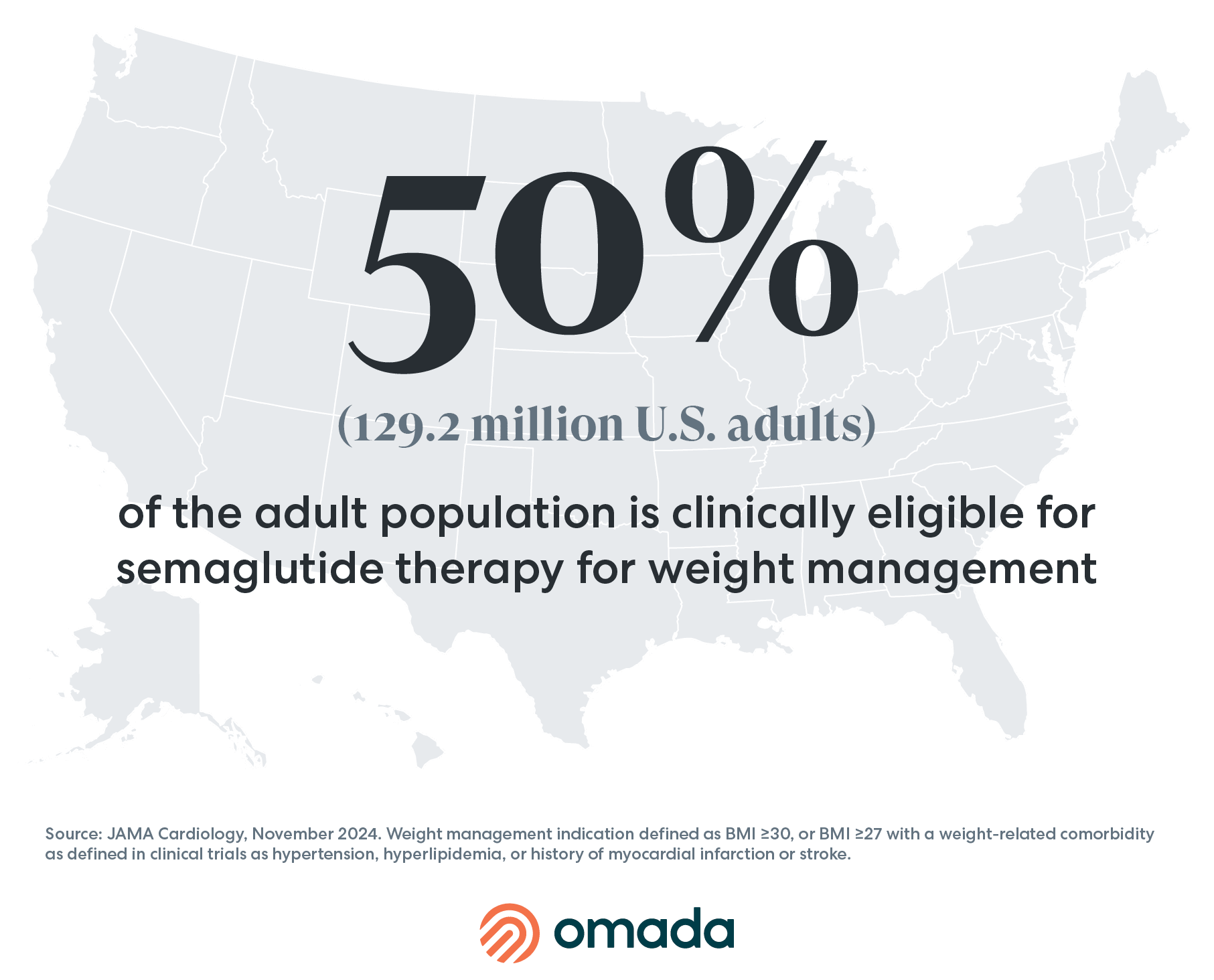
While GLP-1s have been effective in managing type 2 diabetes for more than a decade, their emergence as a breakthrough therapy for obesity put the medications on the map. The latest research from JAMA Cardiology estimates that 129.2 million U.S. adults (or half of the country’s adult population) are eligible for semaglutide therapy for weight management alone. However, over the last year, GLP-1s have been approved to treat conditions beyond diabetes and obesity, including cardiovascular disease, obstructive sleep apnea, and most recently, chronic kidney disease.
Additional indications may be on the horizon, such as metabolic dysfunction-associated steatohepatitis (MASH)—formally known as NASH—which currently has multiple treatment candidates in phase 3 trials. Other indications include, Alzheimer's and Parkinson's disease, substance and alcohol use disorders, and obesity-associated cancers.
As these revolutionary medications gain FDA approval to treat an array of conditions, more people will meet eligibility requirements. As a result, pressure on payers and employers will continue to increase as patients struggle with unaffordable list prices, costing between $499 and $1,000 for a monthly supply.
A: Demand for GLP-1s is pushing more employers to offer coverage. In May 2024, a survey by the International Foundation of Employee Benefits revealed that one-third of U.S. employer health plans now cover GLP-1s for diabetes and weight loss, up from 26% in 2023. On average, GLP-1s for weight loss accounted for 9% of employers’ overall annual medical claims spending in 2024, indicating significant pressure to manage these costs strategically in 2025. Companies may benefit from assessing their GLP-1 strategy alignment with business goals and employee health needs.
A: Successful strategies include providing support through specialized lifestyle behavior programs like Omada's Enhanced GLP-1 Care Track. Such programs support behavior change, encourage physical activity, and provide nutrition coaching, helping individuals lose and maintain their weight after discontinuing the medication. Recent four-month findings suggest that members participating in the Enhanced GLP-1 Care Track experienced 28% greater average weight loss than those on GLP-1s who were not in the Enhanced GLP-1 Care Track, and post-discontinuation, Enhanced Care Track members in the discontinuation path maintained their weight, with a -0.1% average weight change according to new data from Omada Insights Lab.
Early Outcomes of Omada’s GLP-1 Enhanced GLP-1 Care Track
Through the ANSWERS Initiative, the Omada Insights Lab studies the impact of behavior change coupled with GLP-1s to identify effective interventions. Our 2024 analyses highlight the complexity and emotional nature of the GLP-1 member journey, and show that when members combine GLP-1 therapy with Omada’s Enhanced GLP-1 Care Track, they can achieve healthy weight loss and health benefits.
A: According to the study Early GLP-1 Care Outcomes: Setting the Stage for Long-Term Weight Health, individuals in the Enhanced GLP-1 Care Track achieved a remarkable 28% average greater weight loss compared to those who met similar eligibility criteria and were not in the Care Track. This result was statistically significant (p<0.001), indicating that tailored GLP-1 support can be effective in boosting weight loss outcomes.
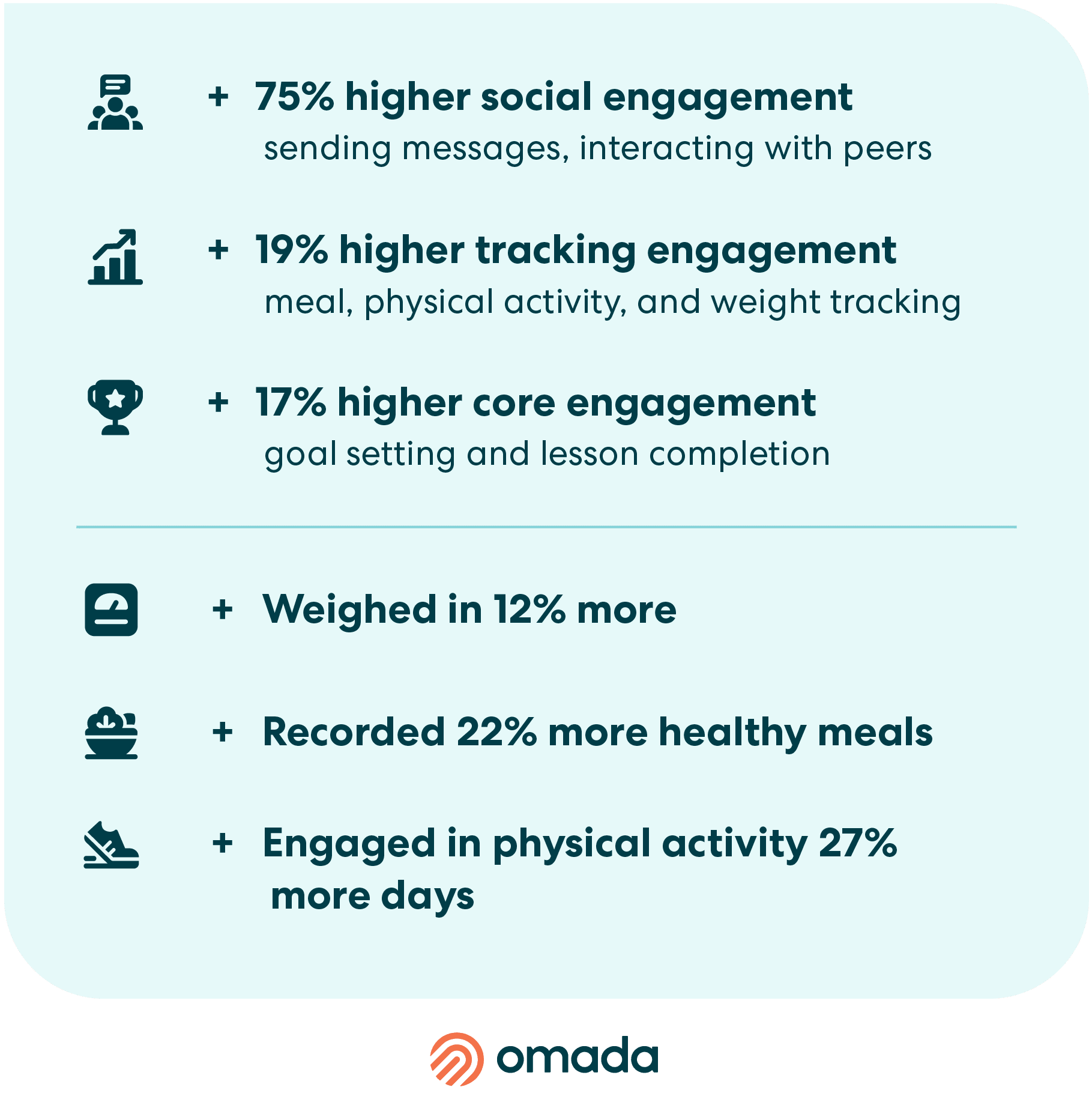
A: Participants in this care track reported a 12% average increase in self-efficacy at four months (p=0.01) compared to baseline, and expressed increased confidence in their ability to lose weight. Additionally, on average, members in this track were approximately 22% more engaged than members who met similar eligibility criteria and not in the track, which is a critical component to help members maintain focus and motivation throughout the weight loss journey.
Maintaining Weight Loss After GLP-1 Discontinuation
A: A recent analysis revealed that 84% of Omada members in the GLP-1 discontinuation path within the Enhanced GLP-1 Care Track experienced less than a 4% weight gain 16 weeks after discontinuing GLP-1 therapy. Moreover, members who opted into this discontinuation path showed a minimal average weight change of -0.1% during the same period, highlighting the potential for successful weight maintenance after GLP-1s with specialized, tailored support.
A: In an Omada member survey, 75% of respondents stopped using GLP-1 due to access-related issues, including cost, loss of insurance coverage, and drug shortages. These barriers are significant hurdles in maintaining the treatment, impacting the ability of many individuals to continue their weight management efforts.
A: Yes, among a subset of surveyed members (n=83), 86.7% expressed a desire to continue losing weight, while 13.3% aimed to maintain their current weight. This demonstrates members’ commitment to achieving weight management goals, even after discontinuation due to external factors.
A: The ongoing research by Omada Insights Lab’s ANSWERS Initiative underscores the importance of addressing access and affordability barriers so that these beneficial GLP-1 therapies can be available to all. They also demonstrate the promising potential of specialized tailored support in helping individuals achieve and maintain long-lasting weight loss.
Primary Care Perspectives on Third-Party Prescribing
A new survey by Omada Health collected data from 2,000 primary care physicians (PCPs) to understand their experiences prescribing GLP-1s to patients, as well as their points of view on third-party telehealth prescribers. Over the last two years, telehealth companies have capitalized on the GLP-1 boom by creating prescribing networks to expand accessibility, and prescribe compounded formulations. According to the survey, 64% of PCPs actively advised against patients using third-party telehealth prescribers to obtain their GLP-1 medications, with 50% listing continuity of care as a primary concern.
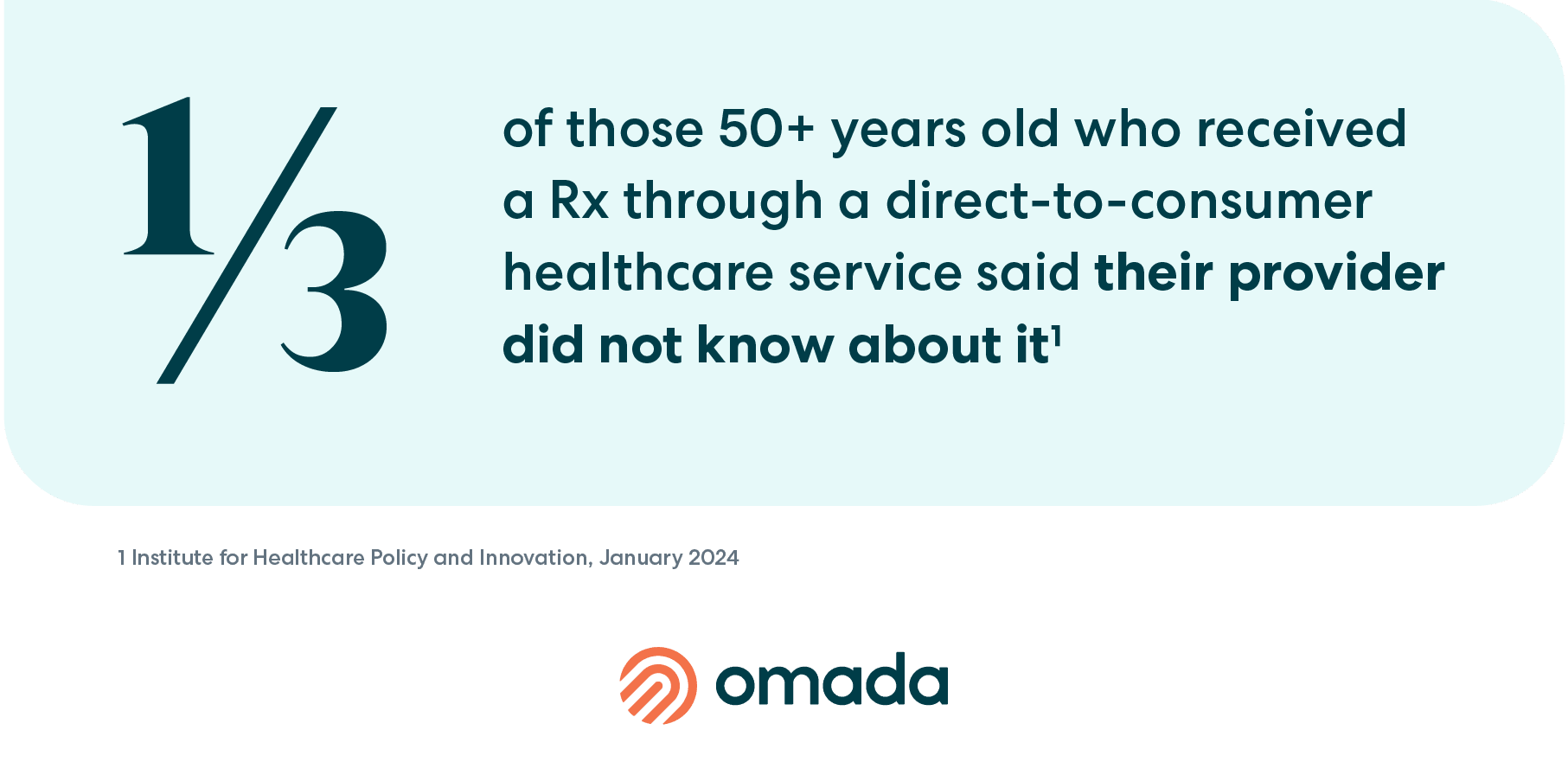
A: Third-party telehealth prescribers are gaining in popularity for their more-convenient access to GLP-1s. However, this approach lacks coordination with the individual’s primary care provider. In a recent poll, one-third of older Americans stated that their doctor was not made aware of the new medication they were prescribed. Similarly, Omada’s survey found that 61% of PCPs agree or strongly agree that patients don’t always tell them when they get a GLP-1 prescription for weight loss from a third-party telehealth prescriber. This phenomenon may compromise continuity of care and introduce patient safety concerns, including:
Lack of Context to Comorbidities
Comorbidities are likely common in populations taking GLP-1s for weight loss. Those with obesity have more than a six-times increased risk of type 2 diabetes and ~60-70% prevalence of dyslipidemia compared with patients of clinically normal weight. These known risks require a whole-person approach to care from a primary care provider with visibility into the person’s long-term medical history.
Risk of Medication Interactions
When asked about concerns of third-party GLP-1 prescriptions, 43% PCPs reported concerns of medication interactions and or side effect management, while 56% were concerned by overprescribing.
GLP-1s slow the digestion of food, which means they can also affect the absorption of oral medications. There are also some medications that have weight-based dosing, and considering the rapid weight loss associated with GLP-1s, patients require close monitoring to ensure that other medications are dosed correctly. Keeping prescriptions in the medical home may encourage the safe and proper use of GLP-1 medications.
Unknown Contraindications
Critical contraindications of GLP-1s are a history of thyroid cancer and/or hypersensitivity to the ingredients in the medication, meaning if a patient has a history of either of these conditions, the physician should not prescribe the medication. These are important considerations for any physician prescribing GLP-1s.
Want to learn more about GLP-1s and how to manage coverage? Visit our Enhanced GLP-1 Care Track page.