Lower Acute Healthcare Utilization Associated with Virtual Cardiometabolic Health Programs
Lower Acute Healthcare Utilization Associated with Virtual Cardiometabolic Health Programs
Susan M. Devaraj PhD, MS, RD, LDN, Jenna Napoleone, PhD, MPH; Madison Noble, MPH; Christina M Parrinello, PD; Carolyn Jasik, MD; Sarah Linke PhD, MPH
Background:
Type 2 diabetes and hypertension are common and costly conditions that increase risk for hospitalization. Lifestyle-focused virtual health programs may offer an effective and accessible self-management solution for these conditions and reduce future high-cost acute care encounters. The purpose of this study was to evaluate the differences in inpatient and emergency room (ER) healthcare utilization between patients enrolled in a virtual health program (VH) for cardiometabolic lifestyle management vs. usual care (UC) controls at 6 and 12 months.
Methods:
We conducted a real-world, retrospective secondary analysis of healthcare claims incurred between July 2019 and May 2023 from multiple payers. Inclusion criteria included continuous coverage for ≥6 months pre- and post-index, an age range of 18-64 years, and having commercial insurance. Index date was defined as the program enrollment date for VH patients or an outpatient claim with a type 2 diabetes and/or hypertension diagnosis code for UC patients. VH patients were enrolled in Omada for Diabetes (DM; n=317), Hypertension (HTN; n=1,102), or DM+HTN (n=315) program and 1:3 propensity score matched (demographics, clinical characteristics and pre-index costs) to UC controls (n=951, n=3,306, and n=945, respectively). Mean differences in post-index inpatient, ER, and acute (inpatient+ER) encounter counts were compared at 6 and 12 months using t-tests.
Results:
After matching, the VH and UC groups had no statistically significant differences in pre-index characteristics. VH patients across all programs had fewer inpatient, ER, and acute encounters at 6 and 12 months vs. UC (absolute mean difference range -0.01 to -0.33, relative difference range: -5% to -63%). Specifically, DM VH patients had 63% lower inpatient utilization at 12 months, 46% lower ER utilization at 6 months, and 54% and 52% lower acute utilization at both 6 and 12 months vs. UC (all p<.05). HTN VH patients experienced significant reductions at both 6 and 12 months for ER and acute utilization vs. UC (ER: -56%, -43%; Acute: -51%, -40%; all p<.05). Finally, DM+HTN patients had 43% lower ER utilization at 6 months vs. UC (p=.04).
Conclusion:
Using a lifestyle-focused virtual health program to support cardiometabolic disease management may lead to meaningful reductions in high-cost acute care encounters, indicating the value of using virtual solutions as an effective and accessible approach to between-visit care.
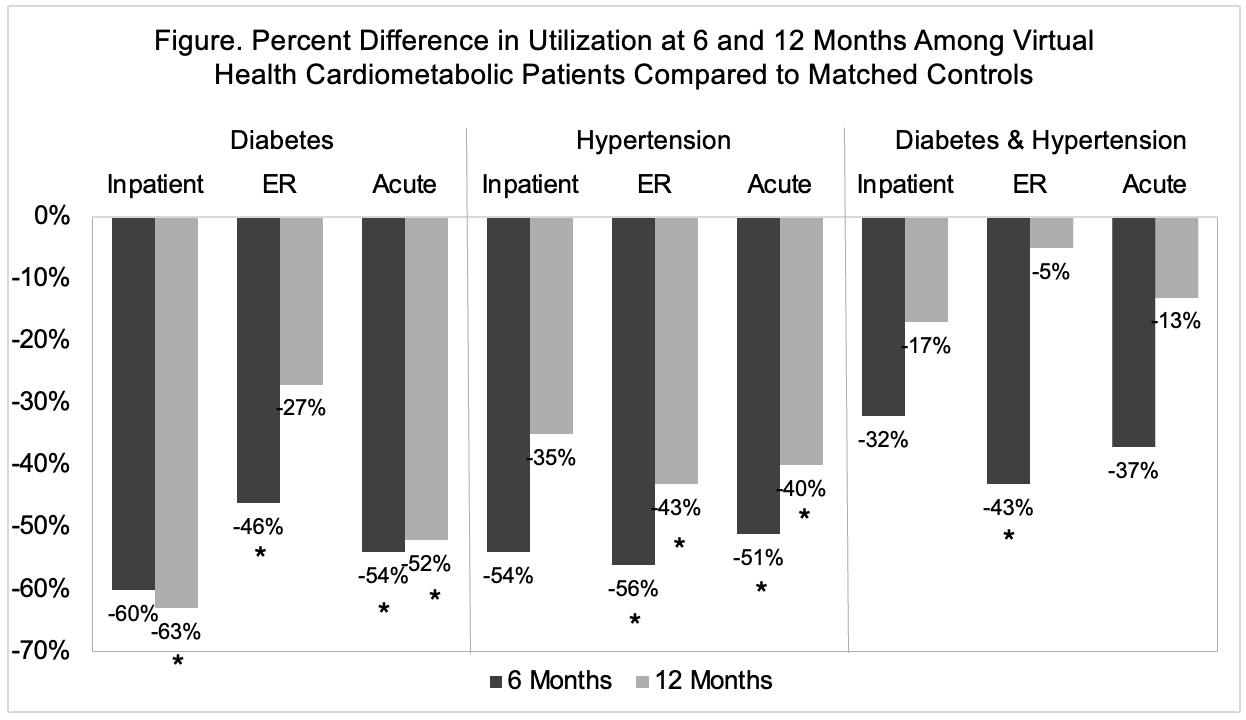
Relative differences in mean encounter counts were calculated as ([(VH - UC) / UC] * 100).
Findings presented at AHA EPI|Lifestyle Scientific Sessions 2025
