How Social Support Influences Weight Health for GLP-1 Users

By Jennifer Becker and Michael Kahn
This edition covers:
- How social support complements health coaching
- The importance of communities in virtual care
- How social support impacts GLP-1 weight health outcomes
As the healthcare industry innovates to maximize the GLP-1 experience for patients, there appears to be an important factor that’s arguably under-discussed: loneliness. At Omada Health, 53% of members entering the Prevention Program felt that getting healthy is a lonely experience. We also know that obesity presents unique challenges for people, given the harmful stigma and discrimination it engenders. GLP-1s are addressing some of the problems commonly associated with obesity, but not all. Researchers worry GLP-1s may actually intensify obesity stigma.
In the U.S. Surgeon General’s “Our Epidemic of Loneliness and Isolation” report, he refers to social connection as “an important social determinant of health, and more broadly, of community well-being, including (but not limited to) population health.” But does the importance of social connection receive the attention it deserves both generally, and in the context of evolving weight health discourse?
Similar to figures we see with Omada members entering the Prevention Program, according to a study commissioned by Cigna, more than half of U.S. adults experience loneliness; and that figure reaches 77% among those with fair or poor physical health. Loneliness also heaps costs on U.S. businesses to the tune of $154 billion annually in stress-related absenteeism. Perhaps unsurprisingly, mounting evidence also suggests that the 42% of U.S. adults living with obesity are lonelier than the general population.
With that in mind, what role can and should social support play in modern obesity care plans? To learn more, we delved into the scientific literature, looked at research from the Omada Insights Lab and interviewed Omada Health coaches Kirby Beal and Joanna Potter, and clinical specialist Jodi Moravec.
Social Support vs. Health Coaching: What’s the Difference?
Omada’s human health coaches are the backbone of our virtual care programs. Members who regularly chat with their coach lose twice as much weight as those who don't. However, we also know that members crave community. A 2019 Omada consumer landscape survey revealed that 36% of people would want a community of like-minded individuals for social support if a virtual care program were offered to them.
Both health coaching––one-to-one support between coach and members––and social support––via peer communities––offer real value to people on their health journeys. Health coaching has been shown to improve quality of life, self-efficacy, and even depression among chronic illness populations; and social support from peers is associated with losing weight and lowering BMI levels in individuals with overweight and obesity.
When offered together, health coaching and social support can help to provide a more comprehensive experience that people need in managing their weight health. That’s why Omada provides access to coaching and social support through topic-based communities. Members who engage with their coach or community in the first week of their Omada program are 24% more likely to be engaged at month four versus those who didn’t have the same social interactions.
“As a coach, I often promote topic-based communities to members who have challenges I simply can’t relate to, such as navigating the daily realities of shift work,” Beal, who also moderates the “Discover Healthy Cooking Community,” said. “I give resources, but it’s often talking to people in these communities, like the ‘shift work’ group, who understand their struggles that can help the most.”
“One post I saw recently was, ‘I’m new to this community and this was a little piece I was missing from Omada,” Potter, who moderates a “Vegetarian & Cooking Nutrition” community, added.
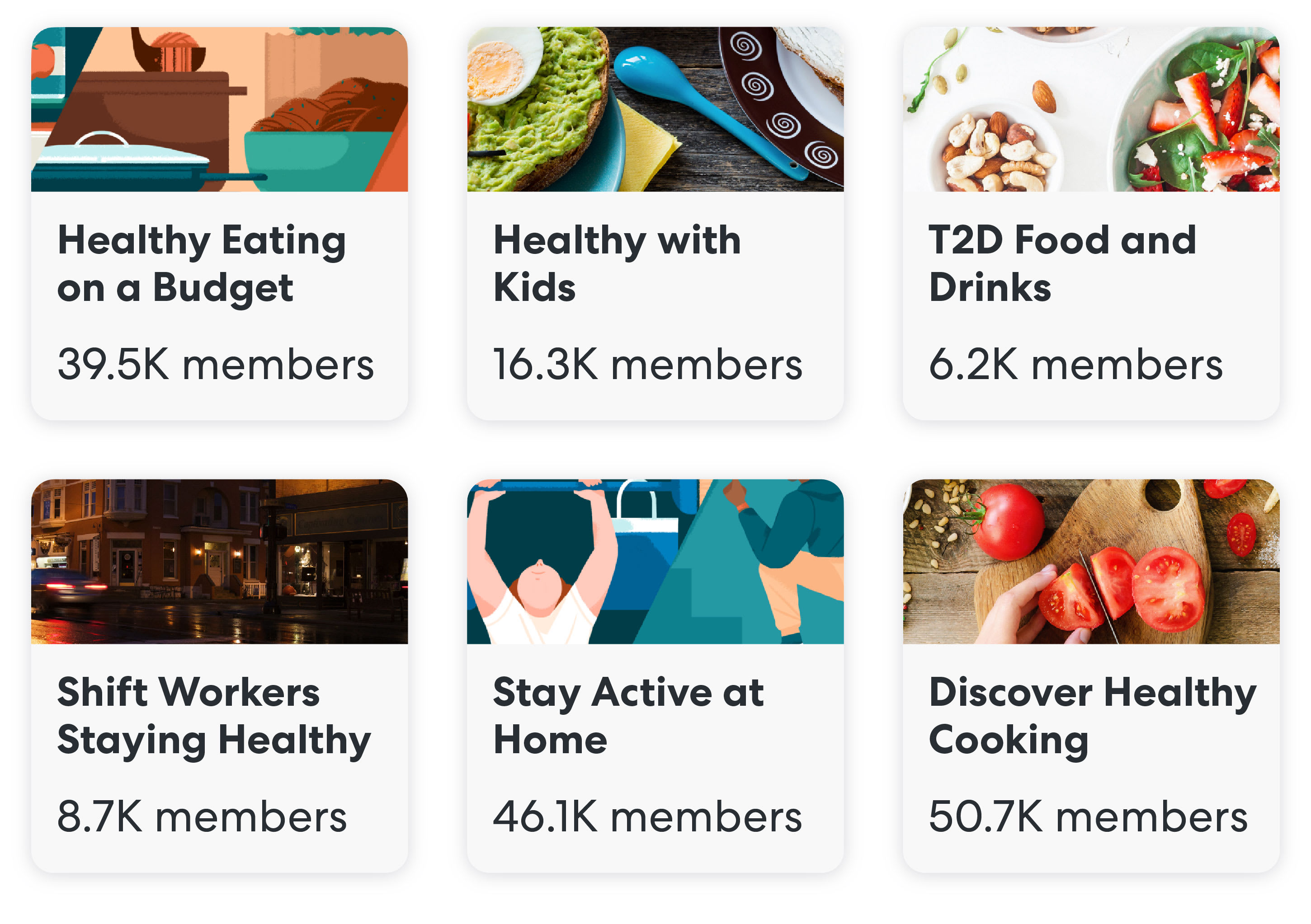
*Figures indicate all-time members
Topic-Based Communities Differ from Other Online Groups
All of Omada’s topic-based communities are are moderated by health coaches like Beal or Potter, or clinical specialists like Moravec. The role of moderators, according to some studies, may play a critical role in maximizing the benefits and safety of online communities built around peer support. Some researchers believe the positive impact of continuous moderation might also direct future research on the potential risks of unmoderated online communities.
As moderators, Omada coaches and clinical specialists have the expertise to combat health misinformation, which researchers refer to as an “emerging public health issue,” in their topic-based communities. They can distribute clinically-validated health resources and tactfully address any inappropriate statements. “But it’s often about stepping back and realizing that [members] like to lead,” Potter said. “We will post, ask questions and guide when needed, but they like to be in charge and lean on the shared experiences of one another.”
Beal and Potter also shared that, in their role as moderators, they help foster a supportive atmosphere by setting community-wide goals and giving kudos to members. The unique context of accessing Omada as an employee benefit, they feel, is another key differentiating factor of these topic-based communities.
“It means there’s already more accountability than, say, in a Facebook group,” Beal told us. “After all, most of the members are getting access to this community through work and want to act appropriately.”
Why Social Support is Critical for GLP-1 Users
Last year, Omada launched a “Medication and Healthy Weight Loss” topic-based community that has exceeded 4,000 all-time members. Jodi Moravec, an Omada Health coach and CDCES cardiometabolic specialist who moderates the community, said one of the first consistent themes to emerge among participants was a collective shame around medication and weight loss.
“They have been shamed often,” Moravec said. “Many haven’t told family or friends about taking GLP-1s because they feel they would be shamed for it. Many have even been shamed by doctors. There are a lot of things going on emotionally. They express that the support and safety of this community is important.”
This community, Moravec said, allows members to gain and share helpful, practical guidance. Members post and comment about GLP-1 side effects, how to discuss prescriptions with physicians, bridging GLP-1 supply shortages with safe FDA-approved alternatives, and encouraging one another to exercise alongside medication adherence.
Moravec also distributes clinically-validated resources on topics ranging from the GLP-1 injection process and navigating side effects, to avoiding weight regain.
“A lot of the engagement in the community, both from a peer-to-peer standpoint and resource sharing from a moderator, are the kinds of things that would be a call into doctor’s offices where they and nurses may not have capacity to help,” Moravec said. “Not only that, but these folks that get this in-between visit support may come into in-person appointments more educated and have more efficient visits.”
Social Support’s Impact on GLP-1 Outcomes
According to a recent analysis by Omada Health and Express Scripts, 82% of Omada members on a GLP-1 experienced amplified weight loss. However, some of the most exciting results arise when drilling down on the impact of relationship-oriented engagement, which in addition to health coaching, encompasses key metrics tied to social support, including:
- Posts in topic-based community and group discussion boards
- Liking/hearting posts in topic-based community and group discussion boards
- Commenting on posts in topic-based community and group discussion boards
Omada members who used Wegovy® and/or Saxenda® and were more engaged in Omada for Prevention lost 1.7x the weight than those who used these medications and were relatively less engaged in the program.
Topics like social support serve as an important reminder that virtual care can and should build on in-person care. While in-person care settings are limited by geography, virtual care solutions can bridge physical distance and offer community to people lacking vital social support for a variety of reasons, including coping with obesity and treatment-related stigma. Omada’s topic-based communities also demonstrate that clinically-validated protocols (i.e. health coaches moderating) can lend helpful structure to social support initiatives.
As the between-visit needs of people living with obesity, including GLP-1 users, outpace the dwindling bandwidth of physicians, virtual care will be increasingly needed to fill the gaps in care, particularly amid concurrent obesity and loneliness epidemics.
